Key Facts About Athlete's Foot

Athlete's foot, or tinea pedis, is a common fungal skin infection that loves damp, warm environments. Fungi, which are tiny microorganisms, thrive in these conditions and can cause mild but annoying rashes when they infect the skin. Though typically not dangerous, athlete’s foot can be quite irritating. Symptoms include itching, burning, and redness between the toes or on the soles of the feet. You might also notice peeling or cracking skin, which can sometimes lead to a secondary bacterial infection if left untreated. While athletes are often associated with this condition due to their sweaty feet, anyone can get athlete’s foot. To prevent it, keep your feet dry and clean, and avoid walking barefoot in public showers or pools. If you suspect you have athlete's foot it is suggested you schedule an appointment with a podiatrist for a diagnosis and treatment plan.
Athlete’s Foot
Athlete’s foot is often an uncomfortable condition to experience. Thankfully, podiatrists specialize in treating athlete’s foot and offer the best treatment options. If you have any questions about athlete’s foot, consult with Patrice Antero, DPM from Tuscany Podiatry. Our doctor will assess your condition and provide you with quality treatment.
What Is Athlete’s Foot?
Tinea pedis, more commonly known as athlete’s foot, is a non-serious and common fungal infection of the foot. Athlete’s foot is contagious and can be contracted by touching someone who has it or infected surfaces. The most common places contaminated by it are public showers, locker rooms, and swimming pools. Once contracted, it grows on feet that are left inside moist, dark, and warm shoes and socks.
Prevention
The most effective ways to prevent athlete’s foot include:
- Thoroughly washing and drying feet
- Avoid going barefoot in locker rooms and public showers
- Using shower shoes in public showers
- Wearing socks that allow the feet to breathe
- Changing socks and shoes frequently if you sweat a lot
Symptoms
Athlete’s foot initially occurs as a rash between the toes. However, if left undiagnosed, it can spread to the sides and bottom of the feet, toenails, and if touched by hand, the hands themselves. Symptoms include:
- Redness
- Burning
- Itching
- Scaly and peeling skin
Diagnosis and Treatment
Diagnosis is quick and easy. Skin samples will be taken and either viewed under a microscope or sent to a lab for testing. Sometimes, a podiatrist can diagnose it based on simply looking at it. Once confirmed, treatment options include oral and topical antifungal medications.
If you have any questions, please feel free to contact our office located in Tuscaloosa, AL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
How to Deal with Athlete's Foot
Athlete’s foot is a type of fungal infection that affects the skin on the feet. It is caused when the tinea fungus grows on the foot. It is possible to catch the fungus through direct contact with someone who has it or by touching a surface that is contaminated with it. This type of fungus thrives in warm, moist environments such as showers, locker room floors, and swimming pools. Your risk of getting it may also increase by wearing tight-fitting, closed-toe shoes, or by having sweaty feet.
Symptoms of athlete’s foot include itching, stinging or burning sensations between the toes. You may also experience toenails that are discolored, thick, crumbly, or toenails that pull away from the nail bed.
Your podiatrist may diagnose athlete’s foot by detecting these symptoms or by doing a skin test to see if there is a fungal infection present. The most common exam used to detect Athlete’s foot is a skin lesion potassium hydroxide exam. To use this method, your doctor will scrape off a small area of the infected skin and place it into potassium hydroxide. The potassium hydroxide will destroy the normal cells and leave the fungal cells untouched so that they are visible under a microscope.
There are a variety of treatment options for athlete’s foot. Some medications are miconazole (Desenex), terbinafine (Lamisil AT), clotrimazole (Lotrimin AF), butenafine (Lotrimin Ultra), and tolnaftate (Tinactin). While these options may be able to treat your fungus, it is best that you consult with a podiatrist in order to see which treatment option may work best for you.
In some cases, Athlete’s foot may lead to complications. A severe complication would be a secondary bacterial infection which may cause your foot to become swollen, painful, and hot.
There are ways that you can prevent athlete’s foot. Washing your feet with soap and water each day and drying them thoroughly is an effective way to prevent infections. You also shouldn’t share socks, shoes, or towels with other people. It is crucial that you wear shower sandals in public showers, around swimming pools, and in other public places. Additionally, you should make sure you wear shoes that can breathe and change your socks when your feet become sweaty. If you suspect that you have Athlete’s foot, you should seek help from a podiatrist as soon as possible.
Relief Options for Ingrown Toenails

Ingrown toenails occur when the nails grow into the surrounding skin, leading to pain, redness, and possible infection. While mild cases of ingrown toenails can sometimes improve on their own, more severe or persistent cases often require medical care. A podiatrist can assess the severity of the ingrown toenail and offer specific treatment options. In advanced cases, minor surgical procedures, such as partial or total nail removal, may be necessary to alleviate pain and prevent recurrence. Ingrown toenails that become infected may also be treated with antibiotics, if needed. Early intervention can reduce the likelihood of such complications, especially for patients with diabetes or circulation issues. Regular care from a podiatrist, such as learning how to correctly trim nails and wearing shoes that fit properly, can also help. If you have a painful ingrown toenail, it is suggested that you schedule an appointment with a podiatrist for an exam and treatment.
Ingrown toenails can become painful if they are not treated properly. For more information about ingrown toenails, contact Patrice Antero, DPM of Tuscany Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
Ingrown Toenails
Ingrown toenails occur when a toenail grows sideways into the bed of the nail, causing pain, swelling, and possibly infection.
Causes
- Bacterial infections
- Improper nail cutting such as cutting it too short or not straight across
- Trauma to the toe, such as stubbing, which causes the nail to grow back irregularly
- Ill-fitting shoes that bunch the toes too close together
- Genetic predisposition
Prevention
Because ingrown toenails are not something found outside of shoe-wearing cultures, going barefoot as often as possible will decrease the likeliness of developing ingrown toenails. Wearing proper fitting shoes and using proper cutting techniques will also help decrease your risk of developing ingrown toenails.
Treatment
Ingrown toenails are a very treatable foot condition. In minor cases, soaking the affected area in salt or antibacterial soaps will not only help with the ingrown nail itself, but also help prevent any infections from occurring. In more severe cases, surgery is an option. In either case, speaking to your podiatrist about this condition will help you get a better understanding of specific treatment options that are right for you.
If you have any questions please feel free to contact our office located in Tuscaloosa, AL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Ingrown Toenail Care
An ingrown toenail is a toenail that grows sideways into the nail bed, causing pain and swelling. Ingrown toenails can worsen and cause drainage, turning into a serious infection.
Several factors affect whether a person is at risk from an ingrown toenail. The many causes include being overweight, diabetes, participating in sports, having a fungal infection of the toe, and cutting your nails too short. Ingrown toenails also have a genetic predisposition, causing some people to be more prone to receive the condition than others. Other causes include improperly fitting shoes and shoes that keep the feet damp.
Ingrown toenails can be preventable with certain measures. For starters, allowing your toe nails to grow slightly longer in length will help prevent them from becoming ingrown. If you have already developed an ingrown toenail, soak the affected toe in warm water. This will alleviate the pain and help prevent an infection from forming. Antibiotic soap or Epsom salts may be added to further help the relieving process and avoid infection. Placing cotton beneath the affected area is also suggested, as this may help the toenail grow upwards and not into the nail bed. Swelling and redness can be reduced by resting with your feet elevated.
A podiatrist should be seen if the pain becomes so serious that it prevents you from doing your everyday activities. If a red streak running up your leg appears or if you suspect your infection has spread, contact a podiatrist immediately. Fast treatments can be undertaken to lessen your pain and have you walking comfortably.
An ingrown toenail can be easily treated with a Band-Aid. Simply wrap the affected toe with a Band-Aid to prevent infection and keep the nail from growing out at a painful angle.
In more serious cases, your podiatrist may decide to make a small incision to remove a portion of your toenail. To prevent the nail from growing back, medication will be placed directly into the nail bed. This procedure would be performed under local anesthesia and is a faster method to alleviate discomfort from an ingrown toenail. Post-procedure directions will have you stay off the affected foot for a day. Afterwards, normal activities can be resumed.
Wound Care for Diabetic Foot Ulcers

Diabetic foot ulcers are a common complication for people with diabetes. They are caused by issues like peripheral neuropathy, poor circulation, and increased pressure on certain areas of the foot. Neuropathy can reduce sensation in the feet, leading to unnoticed injuries that may worsen or become infected. In addition, reduced blood flow slows the healing process, which further increases the risk of infection. Podiatrists are equipped to assess the severity of diabetic foot ulcers and provide appropriate wound care. This includes removing dead tissue, applying specialized dressings, and offloading pressure from the affected area. In some cases, surgery may be required to support the healing process. Proper care is essential to minimize the risk of serious complications, such as gangrene or amputation. By addressing the specific needs of the foot ulcer, a podiatrist can help promote recovery and reduce further risks. If you have a diabetic foot ulcer, it is suggested that you make an appointment with a podiatrist for wound care options.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with Patrice Antero, DPM from Tuscany Podiatry. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact our office located in Tuscaloosa, AL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Wound Care
Diabetics must be wary of all wounds, regardless of depth or size. Diabetes, a chronic disease in which the body cannot properly use glucose the way it normally would, causes various complications that make wounds difficult to heal. Nerve damage or neuropathy will cause diabetics to have trouble feeling the pain of a blister or cut until the condition has significantly worsened or become infected. A diabetic’s weakened immune system can make even the most minor of wounds easily susceptible to infection. Diabetics are also more prone to developing narrow, clogged arteries, and are therefore more likely to develop wounds.
Wounds should be taken care of immediately after discovery, as even the smallest of wounds can become infected if enough bacteria build up within the wound. To remove dirt, wounds should be first rinsed under running water only. Soap, hydrogen peroxide, or iodine can irritate the injury and should be avoided. To prevent infection, apply antibiotic ointment to the wound and cover it with a bandage. The bandage should be changed daily. The skin around the wound may be cleaned with soap.
To prevent further exacerbation, see a doctor—especially if you have diabetes. Minor skin conditions can become larger problems if not properly inspected. As the wound heals, make sure to avoid applying pressure to the affected area.
Finding Relief for Peripheral Artery Disease in the Feet
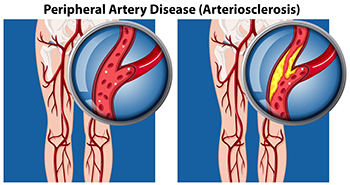
Peripheral artery disease, or PAD, affects blood flow to the extremities, often causing pain, numbness, and discomfort in the feet. To find relief from PAD, managing underlying conditions like diabetes and high blood pressure is essential. Regular exercise, such as walking, can improve circulation and reduce symptoms by encouraging blood flow. Wearing well-fitting, comfortable shoes helps alleviate pressure points and prevent sores. Maintaining a healthy diet and quitting smoking can also significantly benefit vascular health. In more severe cases, medical interventions like angioplasty or surgery might be necessary to restore blood flow. If you have this condition, it is suggested that you are under the care of a podiatrist who can perform regular foot health checks.
Peripheral artery disease can pose a serious risk to your health. It can increase the risk of stroke and heart attack. If you have symptoms of peripheral artery disease, consult with Patrice Antero, DPM from Tuscany Podiatry. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Peripheral artery disease (PAD) is when arteries are constricted due to plaque (fatty deposits) build-up. This results in less blood flow to the legs and other extremities. The main cause of PAD is atherosclerosis, in which plaque builds up in the arteries.
Symptoms
Symptoms of PAD include:
- Claudication (leg pain from walking)
- Numbness in legs
- Decrease in growth of leg hair and toenails
- Paleness of the skin
- Erectile dysfunction
- Sores and wounds on legs and feet that won’t heal
- Coldness in one leg
It is important to note that a majority of individuals never show any symptoms of PAD.
Diagnosis
While PAD occurs in the legs and arteries, Podiatrists can diagnose PAD. Podiatrists utilize a test called an ankle-brachial index (ABI). An ABI test compares blood pressure in your arm to you ankle to see if any abnormality occurs. Ultrasound and imaging devices may also be used.
Treatment
Fortunately, lifestyle changes such as maintaining a healthy diet, exercising, managing cholesterol and blood sugar levels, and quitting smoking, can all treat PAD. Medications that prevent clots from occurring can be prescribed. Finally, in some cases, surgery may be recommended.
If you have any questions, please feel free to contact our office located in Tuscaloosa, AL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Peripheral Artery Disease
Peripheral artery disease (PAD), or peripheral arterial disease, is a circulatory problem in which there is a reduction of blood flow to the limbs due to narrowed arteries. When peripheral artery disease develops, the extremities do not receive enough blood flow; this may cause symptoms to develop such as claudication, or leg pain when walking. The legs are the most common site of peripheral artery disease.
Claudication, or leg pain when walking, is one of several symptoms that can develop due to peripheral artery disease. Other symptoms caused by the disease include painful cramping in the hips, thighs, or calves after certain activities; leg numbness or weakness; coldness in the lower leg or foot; sores on the lower extremities that do not heal; hair loss on the lower extremities; and a missing or weak pulse in the lower extremities. In more severe cases, pain may even occur when the body is at rest or when lying down.
Peripheral artery disease is typically caused by atherosclerosis, a condition in which fatty deposits build up in the arterial walls and reduce blood flow. Smoking, diabetes, obesity, high blood pressure, and high cholesterol are some of the risk factors for peripheral artery disease.
If you are experiencing pain, numbness, or other symptoms in the lower extremities, see your healthcare professional immediately. Diagnosed peripheral artery disease can be treated with various medications, angioplasty and surgery, exercise programs, or alternative medicine. It is important to consult a healthcare professional to determine the best treatment for you.
Exercises Can Improve Foot Health

Engaging in regular exercises focused on the toes, feet, and ankles can significantly enhance foot health and alleviate discomfort. These foot exercises, such as stretching the Achilles tendon, rotating the ankles, and performing heel raises, are beneficial in improving flexibility, strength, and balance. They can be particularly helpful for individuals experiencing foot pain or stiffness. Starting slowly and gradually increasing intensity is advisable, especially for those new to exercise. While these exercises can be done at home, it is wise to consult a podiatrist before beginning any new regimen. A podiatrist can provide personalized advice, ensuring that the exercises you choose are safe and effective for your specific foot condition. This foot doctor can also identify underlying issues that may need professional treatment. If you have problems with your feet, it is suggested that you schedule an appointment with a podiatrist.
Exercising your feet regularly with the proper foot wear is a great way to prevent injuries and build strength. If you have any concerns about your feet, contact Patrice Antero, DPM from Tuscany Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
Exercise for Your Feet
Exercise for your feet can help you gain strength, mobility and flexibility in your feet. They say that strengthening your feet can be just as rewarding as strengthening another part of the body. Your feet are very important, and we often forget about them in our daily tasks. But it is because of our feet that are we able to get going and do what we need to. For those of us fortunate enough to not have any foot problems, it is an important gesture to take care of them to ensure good health in the long run.
Some foot health exercises can include ankle pumps, tip-toeing, toe rises, lifting off the floor doing reps and sets, and flexing the toes. It is best to speak with Our doctor to determine an appropriate regimen for your needs. Everyone’s needs and bodies are different, and the activities required to maintain strength in the feet vary from individual to individual.
Once you get into a routine of doing regular exercise, you may notice a difference in your feet and how strong they may become.
If you have any questions please feel free to contact our office located in Tuscaloosa, AL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.